Are varicose veins causing discomfort and affecting your quality of life?
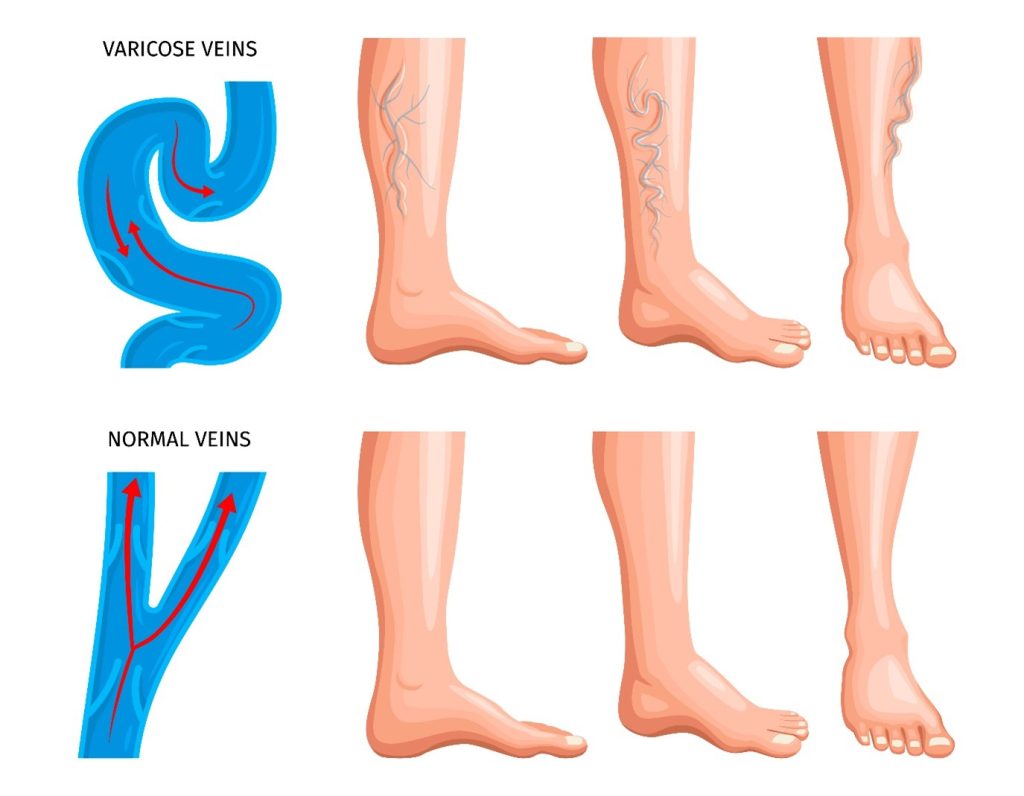
Varicose veins are enlarged, twisted veins that can appear anywhere in the body but are most found in the legs. They occur when the valves within the veins that help prevent blood from flowing backward become weakened or damaged, causing blood to pool in the veins and stretch them out.
Venous insufficiency is a condition that occurs when the veins in the legs are unable to properly return blood to the heart. This can lead to a build-up of blood in the veins, which can cause a range of symptoms such as swelling, pain, and skin changes.
- POTENTIAL RISKS ASSOCIATED WITH VARICOSE VEINS
- Pain and Discomfort: Varicose veins can cause pain, throbbing, aching, and general discomfort in the affected areas. This can impact daily activities and overall quality of life.
- Swelling and Edema: Varicose veins can lead to swelling, particularly in the ankles and lower legs. The accumulation of fluid can cause discomfort and make it challenging to wear certain footwear.
- Skin Changes: Over time, varicose veins may cause skin discoloration and darkening around the affected veins. The skin may appear red, brown, or bluish. In some cases, the skin may become dry, itchy, and more prone to irritation or rashes.
- Ulcers and Sores: In advanced cases, varicose veins can lead to the development of venous ulcers or sores. These are chronic wounds that can be difficult to heal and may require specialized treatment.
- Blood Clots: Although relatively rare, varicose veins can increase the risk of developing blood clots, known as deep vein thrombosis (DVT). Blood clots can be dangerous if they travel to vital organs, such as the lungs, causing a pulmonary embolism.
- Bleeding: Varicose veins close to the surface of the skin may be more susceptible to injury. Even a minor cut or bump can cause significant bleeding due to weakened vein walls.
- Superficial Thrombophlebitis: This condition involves inflammation and blood clots in the veins close to the skin’s surface. It can cause pain, redness, and swelling in the affected area.
- BENEFITS OF THERAPY
Physiotherapy can play a significant role in managing varicose veins by addressing the associated symptoms and improving overall leg health. Here are Benefits of our Varicose Vein Physiotherapy:
✅ Improved circulation and blood flow
✅ Reduction in Swelling, Pain, and Discomfort
✅ Strengthened vein walls and muscles
✅ Enhanced appearance and confidence
- TREATMENTS AND STRATEGIES
- Exercise: Physical activity can improve blood flow in the legs, which can help reduce swelling and discomfort associated with varicose veins. A physiotherapist can develop an exercise program tailored to your needs and fitness level.
- Manual therapy: Massage techniques can help improve blood flow and reduce swelling in the affected areas.
- Education: A physiotherapist can educate you on proper posture and body mechanics to reduce the risk of developing varicose veins or worsening an existing condition.
- Compression therapy: Wearing compression stockings or bandages can help prevent blood from pooling in the veins and reduce swelling. A physiotherapist can advise you on the best type of compression therapy for your condition. Compression stockings are a type of garment that is designed to apply pressure to the legs, ankles, and feet to help improve blood flow and reduce swelling. They are often recommended as a treatment for varicose veins, as well as for other conditions that can cause leg swelling or circulatory problems.

Our Certified Compression garments Therapist can teach you the use of compression stockings by helping you select the right type of compression stocking and ensuring that you are wearing them correctly. Ways that physiotherapy can help include:
- Assessment: A physiotherapist can assess the patient’s condition and determine whether compression stockings are appropriate. They can also recommend the appropriate type of compression stocking, such as knee-high or thigh-high stockings, and the level of compression needed.
- Fitting: A physiotherapist can ensure that the compression stockings fit properly, as stockings that are too tight or too loose may not be effective in improving blood flow.
- Education: A physiotherapist can educate the patient on the proper way to put on and take off the stockings, as well as how long to wear them and when to remove them.
- Monitoring: A physiotherapist can monitor the patient’s progress and make adjustments as necessary to ensure that the compression stockings are working effectively.
Overall, the use of compression stockings in conjunction with physiotherapy can be an effective way to manage swelling and improve circulation in the legs. 👉 Don’t let varicose veins hold you back! Our customized physiotherapy programs are designed to meet your unique needs and provide long-lasting results. 👈

📞 Call now to schedule your consultation to learn more about our proven physiotherapy treatments for varicose veins & embrace healthier legs with our Varicose Vein Physiotherapy services at Helios Physiotherapy and Rehab 🌟
#VaricoseVeins #Physiotherapy #PainRelief #HealthyLegs #Confidence #Wellness #FeelBetter #BookNow #HeliosPhysiotherapy #FollowUs #Instagram #Facebook





